Seeking new health options
Achieving the Sustainable Development Goal of healthy lives and well-being will require fully functional health markets, in which health solutions — whether provided by public or private actors — are affordable and accessible to everyone.
It also requires that stakeholders are able to quickly diagnose and correct where and why health markets break down.
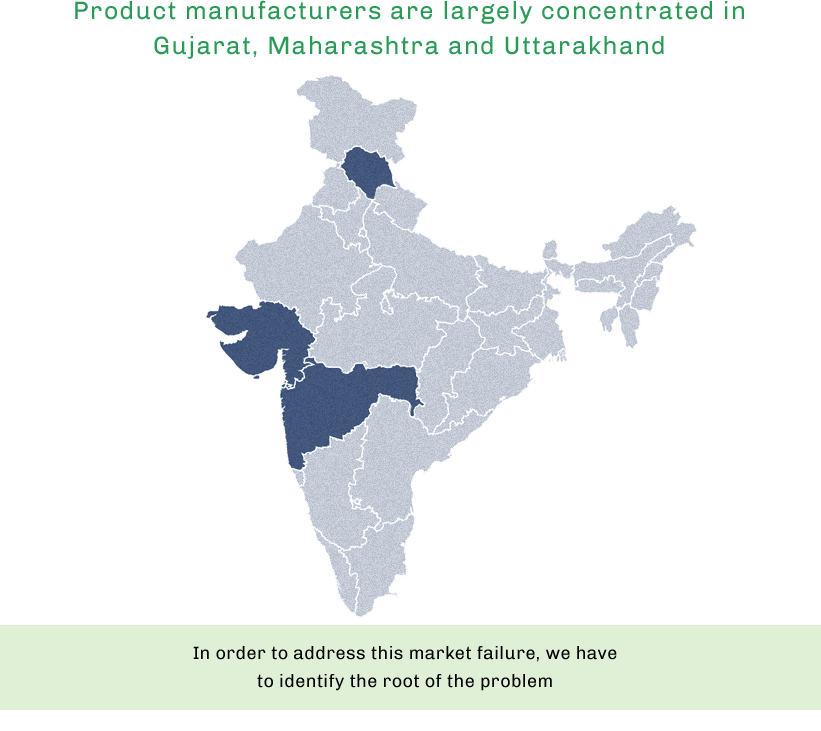
Health market failures are complex — from breaks in the supply chain of medicines or medical products, to a dearth of trained health personnel, to poor policy outcomes, to name only a few. To correct the problems, rather than simply treat the symptoms, close and comprehensive analysis of all market actors is required.
In this interactive feature, Devex outlines one example of how the health market can break down, and how comprehensive analysis can correct it. Join Satya, a recently married 19-year old woman, as she explores family planning options in rural Bihar.
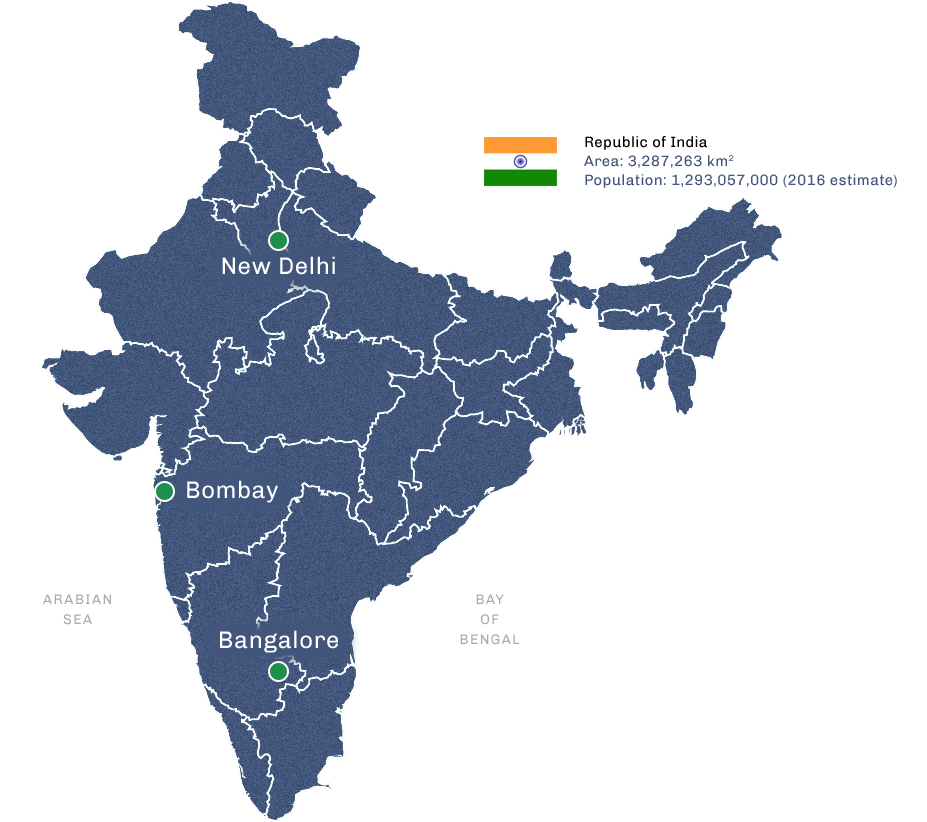
Satya, a recently married 19-year old woman, lives in a rural area in the northern Indian state of Bihar and is looking for family planning methods. Although she married young, she doesn’t want to have children until she’s older.
What are Satya’s options? Explore where health market obstacles occur, and how global development stakeholders can make a difference.
Click here to begin